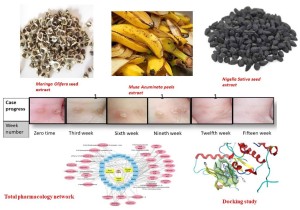
In Vitro and Randomized Controlled Clinical Study of Natural Constituents’ Anti-HPV Potential for Treatment of Plantar Warts Supported with In Silico Studies and Network Analysis
Our new clinical trial study on native plant Moringa olifera and 2 commercial plants was conducted. The aim of this study is to evaluate the anti-HPV potential of a Moringa olifera Lam seed, Nigella sativa L. seed, and Musa Acuminata peel herbal mixture in the form of polymer film-forming systems. A clinical trial conducted in outpatient clinics showed that the most significant outcome was wart size and quantity. Compared to the placebo group, the intervention group’s size and number of warts were considerably better according to the results. Chemical profiling assisted by LC-HRMS led to the dereplication of 49 metabolites. Furthermore, network pharmacology was established for the mixture of three plants; each plant was studied separately to find out the annotated target genes, and then, we combined all annotated genes of all plants and filtered the genes to specify the genes related to human papilloma virus. In a backward step, the 24 configured genes related to HPV were used to specify only 30 compounds involved in HPV infection based on target genes. CA2 and EGFR were the top identified genes with 16 and 12 edges followed by PTGS2, CA9, and MMP9 genes with 11 edges each. A molecular docking study for the top active identified compounds of each species was conducted in the top target HPV genes, CA2 and EGFR, to investigate the mode of interaction between these compounds and the targets’ active sites.
Viral infections play an essential part in human diseases, and recent epidemics due to globalization and the ease of travel have highlighted their prevention as a key concern in protecting public health [1]. Human papilloma virus (HPV) is a common group of viruses that cause skin and genital wart problems in most people [2]. Human papilloma viruses involve different groups and have various epithelial tropisms and life-cycle approaches [3]. HPV infections are categorized as low-risk and high-risk infections [3]. Low-risk HPVs can progress to papillomatosis and, in rare cases, to cancer. However, high-risk HPV is less common but can lead to different types of human cancers, especially cervical cancer, anogenital cancers, and head and neck cancer [3]. The effectiveness of vaccines has been extremely high among young women who were HPV-seronegative before vaccination. However, the nonavalent vaccine can supply additional protection against HPV. Moreover, the notable decrease in HPV among vaccinated women compared with unvaccinated women shows the vaccine to be highly effective [4]. Plantar warts are one type of HPV infection that is caused by an infection in the outer layer of skin on the soles of the feet or hands [5]. When the virus enters through small fractures, wounds, or other vulnerable areas on the bottom of the infected limb, warts form. Plantar warts, which are tiny, scaly growths that appear on the feet or hands, can persist for several years in adults and between a few months and two years in youngsters if untreated [6]. Warts frequently appear on the balls and heels of the feet, as these areas experience the most pressure. Even though these warts are benign, they can cause pain, difficulties walking, and high chances of transmission [7,8]. Patients with warts seek a durable therapy to avoid recurrent visits to physicians. Cryotherapy, electrocoagulation, laser surgery, topical keratolytic, topical antimetabolite drugs, and topical herbal extracts for wart treatment have all been developed. The effectiveness of each of these treatments varies greatly from patient to patient, but recurrence is frequent [9]. Effective therapies remain confronted with difficulties in patient compliance. Herbal medicines and purified natural ingredients are a rich resource for the creation of new antiviral drugs. Because synthetic antiviral treatments are not available against most viral agents, all efforts have been directed toward the discovery of novel pharmaceuticals and complementary/alternative therapies derived from various herbal formulations. Medicinal plants have biochemical and bioactive components that can target specific viruses or heal or prevent a variety of viral illnesses and infections. Natural herbal formulations and compounds derived from plants are widely used as a rich resource for the development of novel antiviral drugs against a variety of viruses, including coronaviruses, influenza viruses, human immunodeficiency viruses, herpes simplex viruses, severe acute respiratory syndrome (SARS) virus, Middle East respiratory syndrome (MERS) virus, and hepatitis B and C viruses. Our study is focused on natural herbal formulas made of Nigella sativa (N. sativa), Musa Acuminata peels (Musaceae), and Moringa oleifera (Moringaceae) that have antiviral activity. Nigella sativa (N. sativa) is a member of the Ranunculaceae family. Seeds and oils have a long history of use in various systems of medicine and nutrition. The presence of thymoquinone, a significant bioactive ingredient of the essential oil, is responsible for the majority of this plant’s medicinal effects. N. sativa contains a variety of phytoconstituents and derived compounds that have a wide range of biological effects, including antioxidant, anti-inflammatory, antibacterial, anti-fungal, anti-parasitic, anti-protozoal, antiviral, cytotoxic, anticancer, and neuro-, gastro-, cardio-, hepato-, and nephroprotective properties. Moreover, traditional medicine uses banana plants to treat viral infections such as measles and chickenpox. Earlier studies have shown that banana peels contain vitamins C, E, and B6 which act as antioxidants, especially vitamin C. Furthermore, Moringa oleifera (Moringaceae) has been used in many traditional therapies and pharmacopoeias to treat a wide range of medical disorders such as malaria, diabetes, skin infections, tuberculosis, anemia, headaches, epilepsy, and sexually transmitted infections, as well as for wound healing. The herb is widely used in African traditional medicine to treat AIDS and related secondary diseases caused by HIV. It shows substantial antiviral activity against viruses such as HIV, HSV, HBV, EBV, FMDV, and NDV. Regarding formulations, several transdermal drug delivery methods and drug targeting formulations at the desired concentration have been studied in previous studies. Precise and efficient film-forming methods have considerable potential for controlling medication distribution through the skin.
A synergistic botanical blend was prepared from Moringa oleifera, Nigella sativa, and Musa acuminata peels methanolic extract with a ratio of 1:1:1. Then, the adhesive film, as an attractive method for a topical and transdermal drug delivery system, was prepared [24,25]. Chitosan and PVA together are known as a very compatible duo that produces good films in terms of its mechanical, morphological, and controlled release characteristics. The herbal PFF showed appropriate thickness for skin application (0.012 ± 0.05 mm) as it was clear and did not affect normal skin appearance, as shown in Figure 1. The folding endurance (70 ± 33) was sufficient for the application’s purpose and timing. The stickiness forces (0.8 ± 0.1 N) revealed a beneficial property that allowed the medication to stay where it was applied for the specified amount of time. Regarding the viscosity of the solution, it was 100 ± 2 cp, which signifies the flowability of the solution on application.
The first clinical examination revealed that the participants had an average of 4 ± 0.4 warts with a diameter of 1.1 ± 0.2 mm. Progress in the clinical signs was supported by episodic photographing showing a reduction in warts remission (number and size). After fifteen weeks, the results significantly differed between the intervention and placebo group in terms of wart size (p < 0.01) and number (p < 0.05).
A comparison between the two groups over 15 weeks in terms of pain and erythema scores using the VAS method. The graph shows a significant difference between the intervention (treated) group and the control group in scores that started at the third week and continued to weeks nine and fifteen. Erythema differs, with a high significant average score, between the two groups (p = 0.0019), while the pain average score shows a significant difference (p = 0.008).
Metabolomic profiling assisted by HR-LCMS analysis of the crude extract Nigella sativa led to the identification of a wide range of secondary metabolites belonging to different phytochemical classes.
This study describes an improved approach for managing plantar warts attributed to causative HPV, which was verified based on photographs of the warts’ size and quantity, and pain and erythema scoring before and after treatment. It has been proven that a novel herbal blend in the form of polymer films can be an effective regimen for improving the skin quality of patients that are impaired by plantar warts. Furthermore, the chemical profiling of Moringa olifera seeds, Nigella sativa seeds, and Musa acuminata peels assisted by LC-HRMS (an HPLC system coupled to a high-resolution mass detector) led to the dereplication of 49 metabolites. Regarding the network pharmacology study, the mixture of the three species identified CA2 and EGFR as the top identified genes related to HPV infection in the studied gene set. Regarding the molecular docking studies, the most active identified compounds of each species showed good fitting and a comparable binding interaction with key amino acid residues bonded to native ligands for both CA2 and EGFR enzymes, the top target HPV genes. In this manner, Nigellidine 1-O-Sulfate, ferulic acid, kaempferol, quercetin, and 9-(4-Hydroxyphenyl)-2-methoxy-1H-phenalen-1-one showed binding energy scores in relation to the CA2 enzyme 1.5–2-fold greater compared to the native sulfonamide ligand (SUA) inhibitor. Quercetin showed a binding energy score in relation to the EGFR enzyme 1.4-fold greater compared to the native erlotinib ligand inhibitor. Supporting this NP study, the most active identified compounds of each species were further in silico studied to assess their gastrointestinal absorption by applying Lipinski’s rule of five and Veber’s rule analysis. The data indicated that this herbal mixture could be a future strategy to combat HPV infections.
